This content material initially appeared on diaTribe. Republished with permission.
By Anna Brooks
On the seek for a kind 1 diabetes treatment, scientists are experimenting with easy methods to engineer beta cells to outlive immune system assaults. On the American Diabetes Affiliation’s 83rd Scientific Periods in San Diego, consultants shared early analysis findings and the place we’re on the trail to stopping kind 1 diabetes.
Researchers, advocates, and sufferers have lengthy looked for a treatment for kind 1 diabetes, a power autoimmune situation through which the immune system destroys insulin-producing beta cells of the pancreas.
Proper now, the closest factor to a treatment is a pancreas transplant or the transplantation of beta cells from deceased donors. Each choices include main caveats, such because the restricted variety of pancreatic organ donors, how sophisticated it’s to guard transplanted beta cells, and the necessity for long-term immunosuppressive treatment.
“To achieve the true management for glucose that sufferers want, we have to discover a treatment,” mentioned Judith Agudo, principal investigator on the Dana-Farber Most cancers Institute. “And a real treatment comes from getting again what’s lacking – the lacking beta cells.”
Agudo was one in every of a handful of consultants who spoke on the ADA’s Scientific Periods and shared what they’re engaged on to crack the beta cell code and different pathways to cease kind 1 diabetes.
Engineering super-strong beta cells
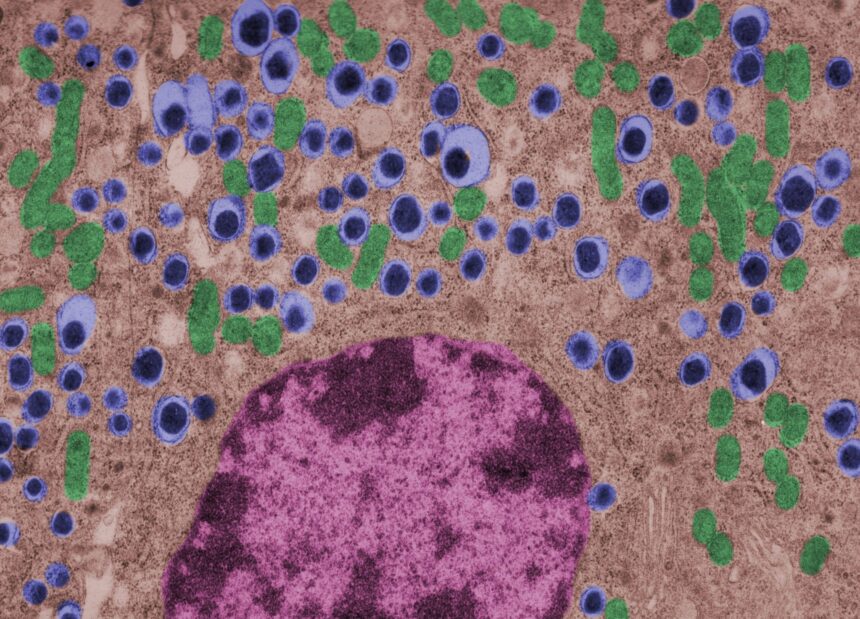
In kind 1 diabetes, the immune system identifies beta cells as overseas. This triggers T-cells (which usually assist shield the physique from an infection) to assault. One technique for coping with that is taking treatment that lowers the physique’s immune response.
The problem right here is that suppressing the immune system makes the physique extra susceptible to an infection and most cancers. Individuals with diabetes are already at the next threat for growing infections and most cancers, so long-term immunosuppression comes with further dangers.
Agudo has been learning mannequin T-cells she created referred to as Jedi T-cells, which allow her to review the immune system’s assault on beta cells. By means of her analysis, she seen that although many cells had been focused by Jedi T-cells, some had been capable of survive.
“We be taught from nature, from cells which might be capable of escape from an immune assault,” she mentioned. “It tells us this can be a wholesome, insulin-producing beta cell that’s dealing with a powerful T-cell assault.”
Whereas the mechanism behind why some beta cells can resist a T-cell onslaught is unknown, Agudo mentioned uncovering this might enable scientists to engineer tremendous sturdy beta cells that may be transplanted into sufferers and survive with out the necessity for medicine that compromise the immune system.
Cloaking beta cells
One other subject is defending cells which have been transplanted. T-cells will establish and assault the transplanted cells simply because it did with the unique cells – so how will we preserve the brand new cells secure?
Agudo defined that one possibility is hiding them. One technique is known as encapsulation, which offers transplanted cells with a bodily barrier that forestalls immune cells from reaching them. The draw back right here is the barrier could make the trade of vitamins and oxygen tougher, in addition to stop the insulin the cells create from entering into the blood.
Different analysis suggests an “immune cloaking” technique the place islets are engineered to cover from or be unrecognized by immune cells that may usually goal them as overseas objects.
“They turn out to be invisible, conceal in plain sight, and now they will survive,” Agudo mentioned.
Utilizing intestine micro organism as a vaccine
Proof from research means that the intestine microbiome is a key part within the improvement of kind 1 diabetes.
Aleksandar Kostic, assistant professor of microbiology at Harvard Medical Faculty and investigator on the Joslin Diabetes Heart, mentioned his analysis round utilizing microbial antigens (invading microbes or overseas substances) to develop a vaccine for kind 1 diabetes.
Present analysis helps the concept of vaccines in opposition to viruses that stay within the digestive tract like Coxsackievirus B, which is considered a consider growing kind 1 diabetes. Latest animal research have additionally been investigating a Salmonella-based vaccine to stop and possibly even reverse diabetes. Kostic’s analysis has centered on vaccinating in opposition to one other microbial antigen referred to as poly-N-acetyl glucosamine, which can result in safety in opposition to the situation.
“We’ve began growing this as remedy for kind 1 diabetes,” Kostic mentioned. “We’re discovering vaccination with this antigen can halt diabetes in mice.”
Researchers like Kostic and Agudo are a part of the ADA’s Pathway to Cease Diabetes program, which offers scientists with grants and assets to speed up and rework diabetes analysis.
“It might sound like science fiction however it isn’t, it’s taking place,” Agudo mentioned. “We’re on the very starting, however it’s actually an thrilling second.”